Precision Fire Protection News
Cutting Edge Microhospitals

Microhospitals, acuity-adaptable patient rooms, and proton therapy centers: A trio of emerging health care components that safety professionals need to know
NO SINGLE THEME READILY connects the trends occurring in today’s health care facilities. Rather, a number of factors, including cutting patient costs, improving access to health care, and relentless technological advancement drive a diverse mix of changes in facility design and health care delivery. Facility managers, first responders, code officials, engineers, architects, and standards organizations like NFPA must stay informed about those changes so that the fire and life safety aspect of patient safety isn’t lost in the mix.
As part of this issue’s focus on health care, NFPA Journal has identified three aspects of health care facilities nationwide that safety professionals need to pay attention to: microhospitals, acuity-adaptable patient rooms, and proton therapy centers. Each of these emerging areas could affect the application of codes and standards, the design and construction process, and emergency response.
In February 2018, the Wall Street Journal published an article titled “What the Hospitals of the Future Look Like.” Topping the newspaper’s examination of these forward-looking facilities were so-called microhospitals. In stark contrast to the expansive, multi-million-square-foot hospital complexes found in many urban areas, microhospitals typically measure anywhere from 15,000 to 60,000 square feet, many of them smaller than a typical supermarket.
Not to be confused with quick- or urgent-care centers, microhospitals are designed to provide a similar breadth of health care as that found in a traditional hospital, but in a smaller space and at a lower cost to patients. “Over the last few years, microhospitals have gained a lot of traction as communities throughout the United States prioritize access to health care,” said Jon Hart, a principal engineer at NFPA and the NFPA staff liaison to NFPA 99, Health Care Facilities Code. They’re especially popular in areas where residents live far from a large hospital, Hart added, such as rural or suburban towns or parts of sprawling urban communities.
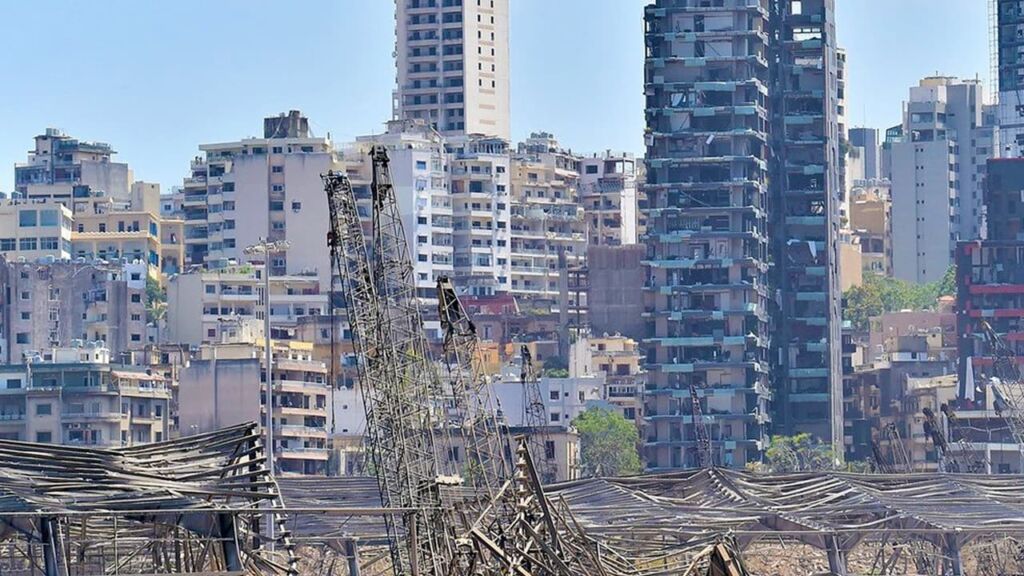
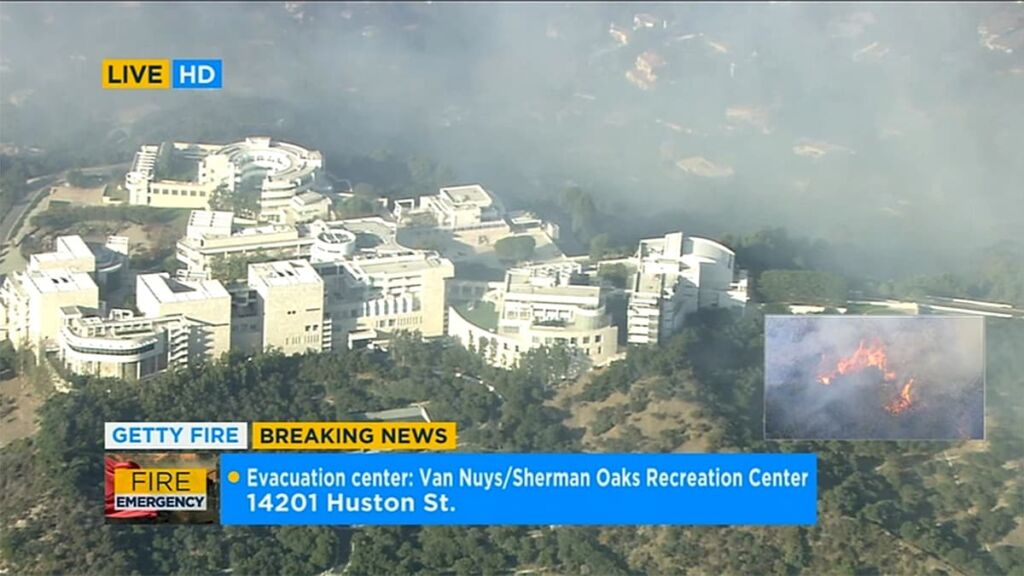
Microhospitals contain the same range of services as conventional hospitals, but with a limited capacity and in a smaller footprint. The facilities can sometimes be mistaken for urgent-care centers. Image Capture: Feb 2018 ©2018 Google
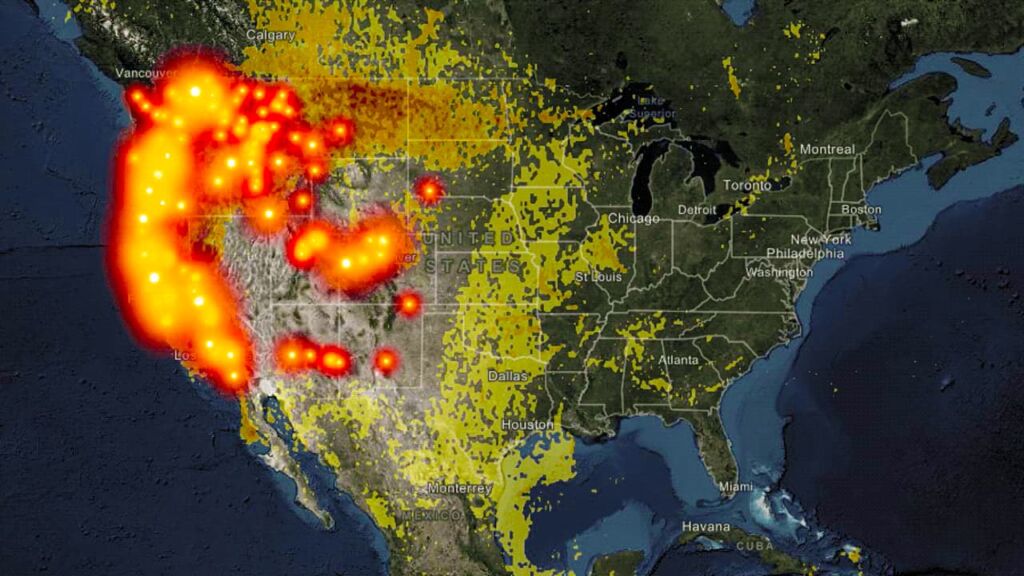
As of December 2017, microhospitals had emerged in 19 states, according to Modern Healthcare magazine. Although the 2018 Hospital Construction Survey—an annual survey of nearly 300 health care facility professionals in the country, conducted by the American Society for Healthcare Engineering of the American Hospital Association’s magazine, Health Facilities Management—found just 3 percent of survey respondents are building or plan to build microhospitals in the next three years, an article published in the magazine in March 2018 reports that “those numbers are expected to spike in the near future.”
With their prevalence expected to rise, it’s important for code enforcement officials, architects, and engineers to familiarize themselves with microhospitals so they understand how to design and classify them, and don’t confuse them with facilities that provide lower-acuity care like an urgent care facility. Microhospitals aren’t specifically addressed in any NFPA codes and standards, nor are there plans to change that, since they’re being treated as traditional hospitals using codes like NFPA 101®, Life Safety Code®, and NFPA 99.
“From the outside, they may look like an urgent care facility, but they should be treated as a traditional hospital and fall under the health care occupancy classification of the Life Safety Code,” Hart said of microhospitals. “They should still be treated like an inpatient facility where patients are expected to be incapable of self-preservation and where they would stay for more than 24 hours.”
Jonathan Flannery, senior associate director of advocacy for the American Society for Healthcare Engineering (ASHE) of the American Hospital Association, echoed Hart’s point in an interview with NFPA Journal. “The challenge is understanding that they have to be built to the same standards as a hospital,” he said. “Patients are staying there for more than 24 hours, and they’re incapable of self-preservation.”
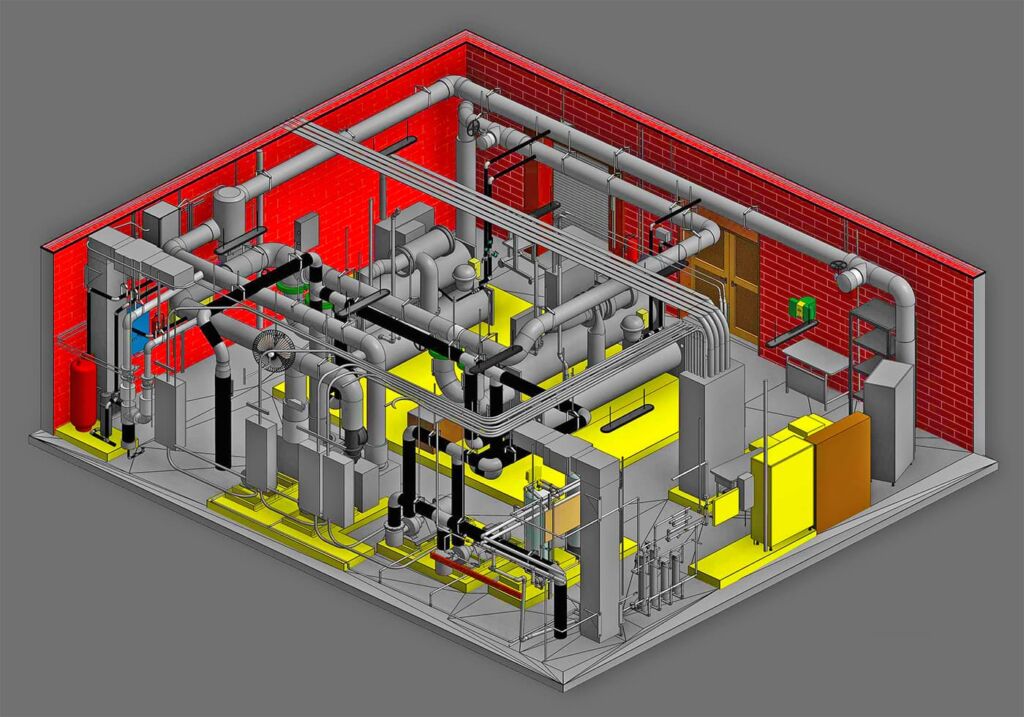
From a construction perspective, Flannery said, architects and engineers need to understand they’re going to have to fit the same types of medical and life safety systems they would put in a traditional hospital into the much smaller footprint of a microhospital. This would include, for example, Category 1 gas and vacuum systems and a Type 1 essential electrical system—in other words, the highest-functioning equipment needed for when failure would result in serious injury or death to patients, according to NFPA 99. “The cost per square foot will end up being higher than you might think,” he said. “But the concept is good.”
On any given day, one in 31 hospital patients nationwide is sick with a health care–associated infection (HAI), also known as a hospital-acquired infection, according to the United States Centers for Disease Control and Prevention (CDC). The CDC estimates that nearly 100,000 patients die from HAIs each year in the United States. Many of these deadly infections can spread as a result of transferring patients from one unit of a hospital to another, such as from an intensive-care unit to a lower-care unit.
To defend against this, acuity-adaptable patient rooms, or rooms in which patients are cared for from admission through discharge regardless of their condition, have emerged as a potential solution. The model can also reduce “errors in communication, patient disorientation, dissatisfaction, and falls,” according to a 2013 article published on acuity-adaptable rooms in the journal Critical Care Nursing Quarterly.
But to meet codes like NFPA 99, Health Care Facilities Code, acuity-adaptable rooms could also mean higher costs for hospitals.
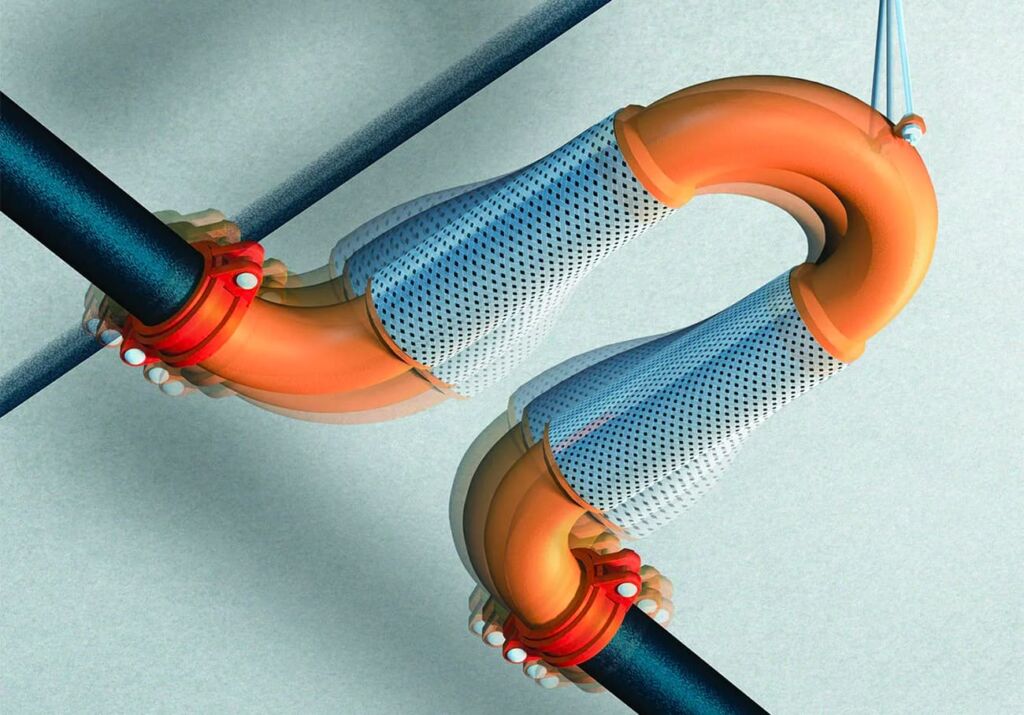
“The application of NFPA 99 is based on risk to patients,” Jon Hart, the NFPA staff liaison to NFPA 99, explained in a blog post early last year. “Rooms with higher-acuity patients, where the risk of a system failure can have significant impacts, require more protection. All rooms designed to accommodate the acuity-adaptable approach will have to meet the requirements for the higher level of risk. This will likely mean a higher number of rooms that need to meet the increased requirements for the higher risk. Some of the impacts this could have would be additional medical gas and vacuum outlets and inlets, increased number of electrical receptacles at patient beds, additional zone valve boxes, and increased loads on the critical branch of essential electrical systems.”
According to Hart, facilities with acuity-adaptable rooms remain uncommon across the country, and the scarcity of statistics on their prevalence underpins that assessment. But more may appear in the coming years. The ECRI Institute, a global nonprofit that researches and aims to improve patient care in hospitals, included acuity-adaptable rooms in its 2018 list of 10 trends hospital executives need to pay attention to. “Hospitals are looking for any way they can limit hospital-acquired infections and other complications that come from moving patients around a facility, so if there’s a framework that can be found to make acuity-adaptable rooms work, it could be useful to the entire field of health care,” Hart told NFPA Journal.
The high cost of creating acuity-adaptable rooms that are code compliant is one reason they haven’t become more popular, said Tim Gee, who has worked with the acuity-adaptable room model as principal of Medical Connectivity Consulting, a health care consulting firm based in Oregon that specializes in medical devices. “You need medical devices and infrastructure like medical gas lines and suction lines to support that higher-acuity patient, and most units don’t already have that,” Gee said. “A single monitor needed to support intensive care unit–level care could cost $40,000.”
While the cost, coupled with staffing challenges, has limited the growth of acuity-adaptable rooms, they do exist in some facilities, most notably specialized ones like cardiac hospitals. “Some specialty hospitals have fully flexible- or variable-acuity units that can go all the way up to ICU-level care and they have the proper devices, gas and suction lines, and all the additional infrastructure required to do that,” Gee said. “It makes all of these rooms expensive, and you need a special situation that makes it practical, such as a specialty hospital that only does heart surgeries.”
Gee said specialized health care facilities are also where he sees this trend growing in the future, rather than in more generalized facilities. “If it’s a specialty hospital, then yes, I would see them absolutely considering acuity-variable rooms, especially for new construction,” he said. “I think a typical hospital may invest in units that can flex to a certain level but not up to the ICU level.”
Similarly, Jonathan Flannery, senior associate director of advocacy for the American Society for Healthcare Engineering of the American Hospital Association, said retrofitting existing facilities’ rooms to make them acuity-adaptable is unlikely to happen, but for new construction it’s a possibility, especially given the steps some facilities are already taking to address a separate, pertinent risk.
“The steps facilities are taking to account for operations during emergencies like natural disasters, such as building their facility with 100 percent electrical redundancy, make it easier to adopt the concept of adaptive locations,” he said. “I worked in a hospital where, during the winter, we needed more intensive-care beds because of respiratory complications and influenza, and it’s those kinds of trends where acuity-adaptable locations become very valuable. The challenge is if you don’t have the infrastructure available, you can’t do it.”
As cancer treatments evolve, so do the facilities needed to accommodate them.
Proton therapy centers are a good example. As more are developed throughout the country, experts stress the need for code officials and first responders to familiarize themselves with these intricately designed, often very large structures.
Proton therapy is a form of radiation treatment used to treat certain cancers, especially in children. During treatment, subatomic particles known as protons are isolated and accelerated into tumors with incredible speed and accuracy. The precision of proton therapy reportedly results in fewer adverse side effects than conventional radiation treatments, which are known to destroy healthy cells in addition to cancerous ones.
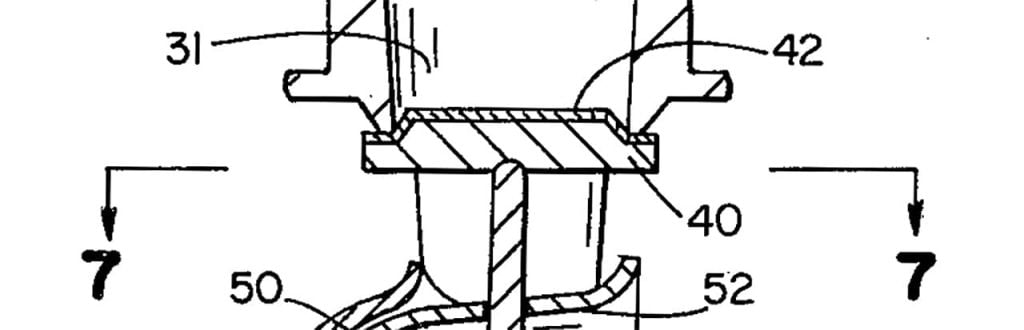
The specialized treatment requires an equally specialized facility to deliver it. Proton therapy centers are usually stand-alone structures composed of equipment weighing hundreds of tons, dozens of miles of cabling, and concrete walls that are several feet thick. The area where the patient receiving treatment lies can rise three-stories high so the massive enclosure surrounding the patient, known as the gantry, can rotate 360 degrees, delivering proton beams anywhere they’re needed.
A 2018 survey conducted by the National Association for Proton Therapy found that the number of proton therapy centers in the United States has roughly doubled in the past four years, with 29 now in operation. “They’re becoming more prevalent, and that’s a trend that’s going to continue,” said Charles Cowles, an anesthesiologist who has experience working at the M.D. Anderson Proton Therapy Center in Houston, Texas. Before attending medical school, Cowles spent 14 years in the fire service.
Cowles knows firsthand the challenges of constructing one of these facilities, and why involvement from code officials is key to making these projects go smoothly.
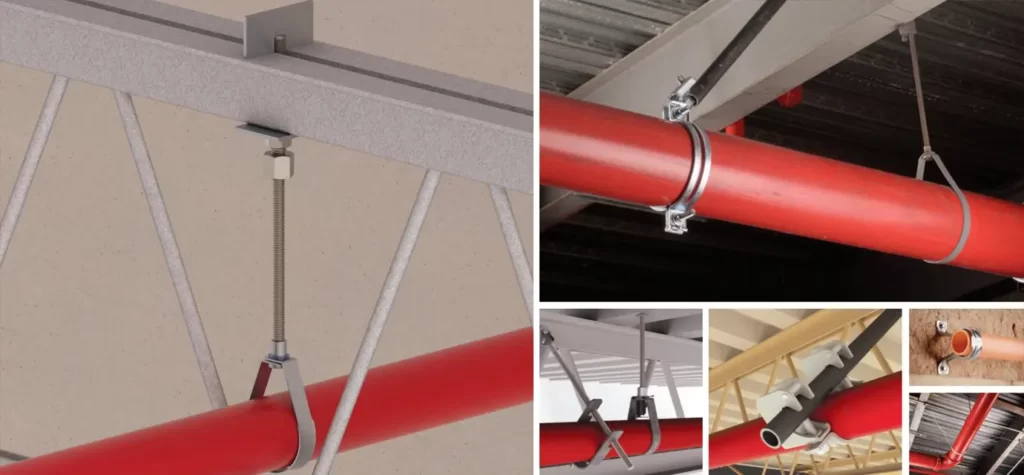
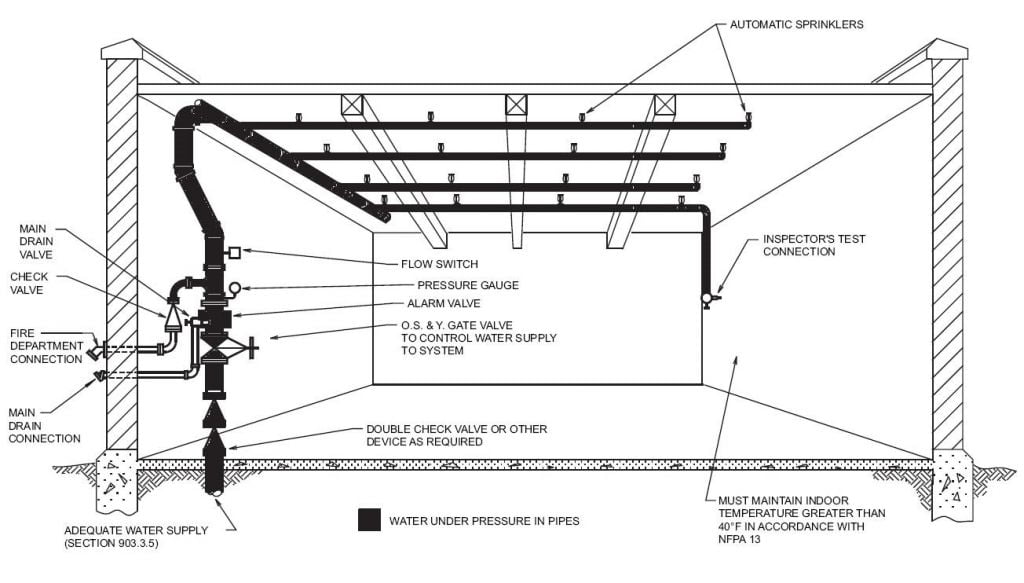
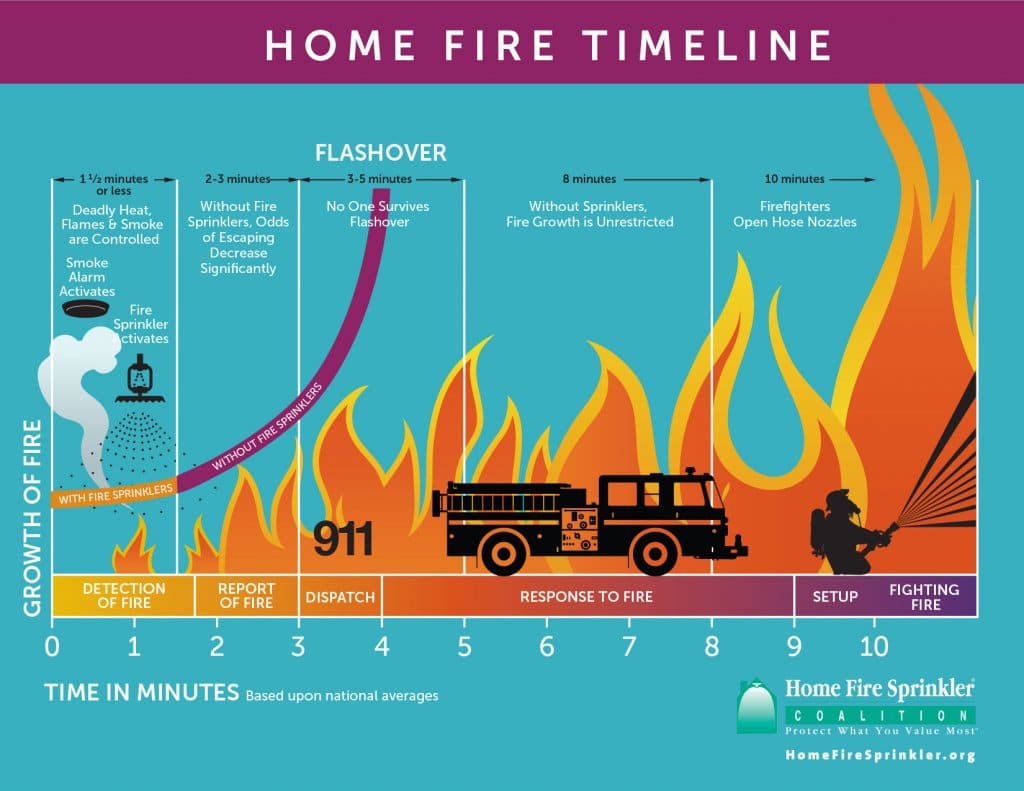
When the M.D. Anderson facility was being built in 2006, doctors didn’t think there would be a high demand for anesthetizing patients, he said, so locations of gas piping for anesthesia weren’t optimized in the layout of the facility—something that can’t be changed now given the nature of proton therapy centers’ construction. “The concrete walls are typically eight feet thick, so there are no modifications that can be done,” Cowles said. “We were one of the first proton treatment centers to be built in the U.S., and if we had to do it over, we would have piped nitrous oxide and waste anesthesia gas disposal and configured the room a bit differently. So it’s important that everybody, especially code enforcement officials, be involved in these projects very early on. It’s not like you can easily add a sprinkler or a pipe or an electrical outlet once it’s completed.”
An article published in October in Health Care Design magazine also stressed the need for involvement and education of multiple groups during the construction of proton therapy centers. “Proton therapy centers need to be built with an attention to detail mirroring the precision of its life-saving treatments,” wrote the authors, who worked on a separate project to build a proton therapy center in Texas. “Because there are so few proton therapy facilities in the country, few contractors and trade contractors have this expertise. The construction team took the time to educate subcontractors and craftspeople on the nuances of this complex project and the critical importance of precision … By creating a collaborative relationship with everyone involved on the Texas Center for Proton Therapy, the project stayed on schedule and the center was able to begin treating patients four months earlier than planned.”
There’s no mention of proton therapy centers in NFPA codes and standards, and no comprehensive guidelines on building or maintaining them appear to exist. Rather, individual components of the facilities are subject to varying requirements, Cowles said. “I would say the front part of the facility can be classified as a business occupancy using NFPA 101®, Life Safety Code®,” he said, adding that guidelines on the treatment area and synchrotron—an extremely powerful source of X-rays—are found in NFPA 801, Fire Protection for Facilities Handling Radioactive Materials, Annex C.8 Particle Accelerators. There are also a number of federal rules governing facilities using radiation.
Outside of the construction challenges, first responders in communities where a proton therapy center is located should waste no time in visiting the facility to familiarize themselves with its unique nature, Cowles said. The gantries where patients receive treatment, for example, have only one way in and one way out, contrary to modern fire safety standards, because of radiation safety standards. Inside the gantries, patients are treated on a table that is suspended a story above the ground, with the gantry rotating around the table, and there are sometimes areas in the gantry where a person could fall through a gap to the ground below. “Both responders and facility staff should become familiar with the facility and realize this is a different environment and responding to an emergency might be difficult,” Cowles said.
Perhaps the most important thing for responders—and anybody at a proton therapy center—to know is where the radiation counter is. Devices such as Geiger counters spin up during treatment and down when treatment ceases, Cowles said. “It’s the only way you can know the treatment room is safe to enter,” he said. “That’s something responders, and anyone at the facility, should get in the habit of assessing. It’s the first thing I check upon entering the treatment room.”
PEOPLE We Protect
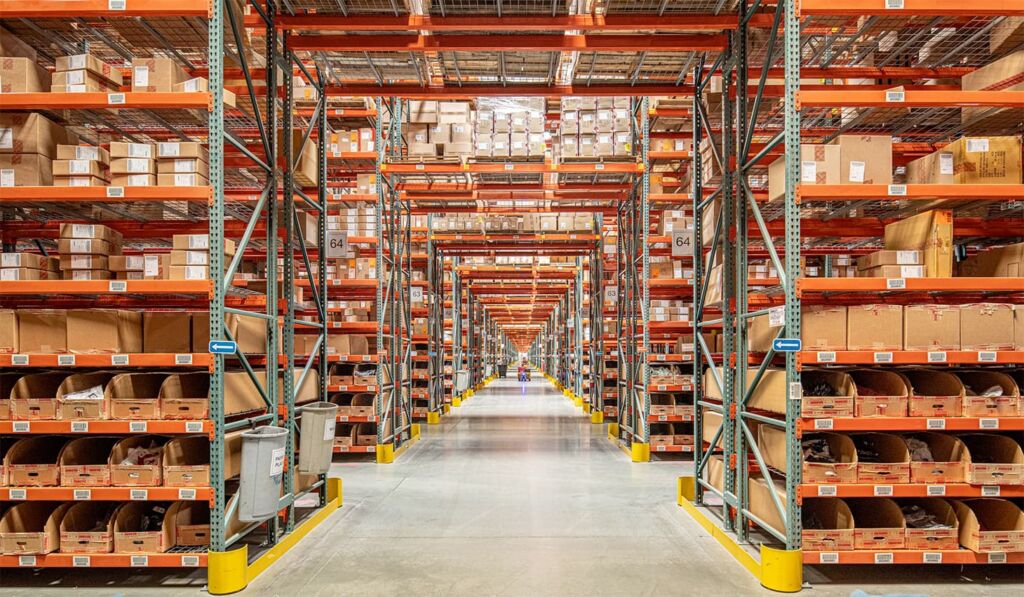
Our Distributors and Suppliers
Experience
Our team started in the fire protection industry over 20 years ago. Since then we have grown into a statewide fire protection construction leader. Our team of project managers, engineers, designers, inspectors, installers, and technicians all share a passion for quality work and high standards. Precision Fire Protection understands the need to complete projects with integrity, safety, and precision!
Dedication
Our mission is to provide our customers with timely, high quality, affordable fire protection services that are guaranteed. We strive to achieve our client’s complete satisfaction. We are relentless in applying the highest ethical standards to ourselves and to our services and in communications with our customers. We aim to fulfill that mission in everything we do.
Precision
Precision Fire Protection keeps its team together, even when it's not. Just as vital as field personnel’s tools are, our project managers are equipped with the latest software to manage projects. Our project managers send dailies, RFIs, and plan revisions to the cloud so that everyone has access no matter where they are. Being connected is our way of ensuring every project goes smoothly.
Safety
Our team of multi-certified managers and supervisors are highly experienced in job safety. Our managers are OSHA certified to handle each project with care and sensitivity to every unique job site. By ensuring on-site safety on every project we work on throughout Southern California, Precision Fire Protection has developed positive relationships with our General Contractors.